Last week I reviewed the issue of antibiotic resistance, and why unlike the perspective held by government, the medical profession and industry, I do not believe the issue is simply a technical problem that can be solved by finding the latest and greatest drug. Such a fantasy underlies much of what unfortunately motivates us as a species, that what we’re looking for is just around the corner, instead of seeing the opportunities all around us. It is this same fantasy that drives drug development, and medical innovation is part and parcel of that which drives the economy, which itself is predicated on limitless, unending growth. The great irony, of course, is that this aspiration of growth is exactly the same as that held by cancer, a disease which is now the leading cause of death in countries such as Canada. But think of the cancer cell for just a moment: ignorant and naive, just a-trying to be the best little cancer cell it can be. It’s all a matter of perspective: on the one hand, a sad story of cancer; but on the other, an inspiring tale about the Little Engine That Could. Where both lead, however, is the same: a state of disorder and destruction. If only the cancer cell could comprehend that it’s story of self-esteem and empowerment destroyed the very foundation of its own existence. The similarities between the behavior of humanity and cancer is striking. It should be no surprise that antibiotic use is associated with an increased risk of cancer (1, 2, 3). Might we consider this a smoking gun?

The inherent entropy that underlies the fantasy of the ‘silver bullet’ can only be addressed by a philosophical reassessment of our values, and what exactly the purpose of medicine is. To my mind, medicine exists for the purpose of alleviating suffering. In ancient India, this ethos is very much reflected in one of the most ancient schools of thought in India called Sankhya. In this atheistic system of philosophy, there is no God to take away your sorrows – you are alone – and yet “you” are also connected to an eternal consciousness. The goal of its philosophy is the alleviation of suffering and the attainment of this super-consciousness – there is no higher purpose. A few thousand years later the historical Buddha proposed a similar idea, that by failing to perceive the temporary and transient nature of our being, we are compelled to act out ignorance, pushed and pulled by our desires and aversions, to create at best a temporary state satisfaction, but one interwoven with perpetual suffering and pain. In ancient India, the historical Buddha was sometimes referred to as the Great Physician, not because he relieved physical suffering, but because his teaching addressed the cause of suffering itself. In this way, modern medicine can never become whole until it addresses these same existential issues, to realize that it exists not to preserve life at any cost, but to preventing and allaying suffering as an inherent virtue.
It can be argued that ignorance is an essential facet of being. But there is a difference between knowing that one is ignorant, versus thinking confidently that one has overcome it. According to the earliest texts, the historical Buddha went out of his way to dismantle the speculative arguments of the know-it-all pundits of his day (e.g. the Tevijja sutta), and freely admitted that there were questions for which there were no answers (such as the origin of the universe – any takers?). Likewise, even in those experiments which are repeatable – the gold standard of science – we cannot be too confident, particularly in the conclusions we draw, as very often we only confirm our biases that are built into the design of the study itself. When it comes to the issue of antibiotic resistance, I think it is very clear that modern medicine does not have a good handle on what is happening, and it’s entire approach to addressing the issue is failing. Sure, things might turn out well if the latest antibiotic proves true, but we have to be honest and admit that this too will likely fail at some point in the future. Thus, we will be confronting the same issue again, but perhaps on an even worse scale, as we experience the blowback that stems from our decidedly adversarial approach. It is our belief that we are separate from bacteria that drives this problem. Instead of a them-vs-us proposition, I propose that we consider the problem of infection as a broader ecological issue, in which the goal is to restore homeostasis and balance.

To achieve this isn’t just a theoretical possibility – there are many examples of homeostatic balance within healthy ecosystems all over the world. Of course, many of these have been destroyed by humans, but some do remain, and exist as a model to follow. There are many things we can learn from studying these ecosystems, and in the myriad interactions between bacteria and other organisms such as plants. Plants, in particular, have been engaged in a slowly evolving chess match with bacteria since the first photosynthetic eukaryotes evolved about two billion years. As such, plants have developed a vast and sophisticated armamentarium in their battle for survival, which includes both utilizing and inhibiting the activities of different bacteria for their own benefit. Many plants in the Fabaceae, or pea family, for example, have evolved an ability to house nitrogen-fixing bacteria within their root nodules, giving them an advantage over other plants that must rely upon soil bacteria for nitrogen fixation. Organic farmers take advantage of nitrogen-fixing plants such as clover and alfalfa to improve the nutrition of the soil. Likewise, herbalists use medicinal plants to the same advantage, utilizing the sophistication derived not just from thousands years of observed use, but from the biochemistry of the plant itself.
 Consider the case of berberine. If you haven’t heard of it before, berberine is a yellow staining isoquinoline alkaloid found in a variety of different plant species including medicinal herbs such as Oregon grape root (Mahonia spp.), goldenseal (Hydrastis canadensis), and goldenthread (Coptis spp.). Berberine is well-known as an effective antimicrobial compound, and while it was never really introduced into clinical practice in the West, it has been used extensively in other parts of the world such as China, sometimes found as an OTC preparation called Huang Lian Su Wan, used in the treatment of GI infection. While berberine is just as good and probably cheaper than many antibiotics, it doesn’t work for all bacteria. Over the millions years of playing evolutionary chess with berberine-containing plants, some bacteria made a play. They couldn’t do anything to stop the toxicity of berberine once it penetrated into the cell, but what they could do is pump it out. Thus, some time in the distant past certain bacteria started to develop specialized pumps in their cell walls, effectively shutting down one of the plant’s primary weapons against bacteria. Just like we are seeing now with antibiotic resistance in medicine, some bacteria became resistant to berberine. The difference is, of course, that this evolutionary chess match between plants and bacteria evolved very slowly. What we have done is isolate the main antimicrobial super-weapons of certain fungi, and then blast away at the bacteria, until like the cybernetic Borg collection in Star Trek, they adapt to our technology and render it useless. Resistance is guaranteed.
Consider the case of berberine. If you haven’t heard of it before, berberine is a yellow staining isoquinoline alkaloid found in a variety of different plant species including medicinal herbs such as Oregon grape root (Mahonia spp.), goldenseal (Hydrastis canadensis), and goldenthread (Coptis spp.). Berberine is well-known as an effective antimicrobial compound, and while it was never really introduced into clinical practice in the West, it has been used extensively in other parts of the world such as China, sometimes found as an OTC preparation called Huang Lian Su Wan, used in the treatment of GI infection. While berberine is just as good and probably cheaper than many antibiotics, it doesn’t work for all bacteria. Over the millions years of playing evolutionary chess with berberine-containing plants, some bacteria made a play. They couldn’t do anything to stop the toxicity of berberine once it penetrated into the cell, but what they could do is pump it out. Thus, some time in the distant past certain bacteria started to develop specialized pumps in their cell walls, effectively shutting down one of the plant’s primary weapons against bacteria. Just like we are seeing now with antibiotic resistance in medicine, some bacteria became resistant to berberine. The difference is, of course, that this evolutionary chess match between plants and bacteria evolved very slowly. What we have done is isolate the main antimicrobial super-weapons of certain fungi, and then blast away at the bacteria, until like the cybernetic Borg collection in Star Trek, they adapt to our technology and render it useless. Resistance is guaranteed.

But not for the patient Oregon Grape root. It was heavily invested in isoquinoline alkaloid technology for the last several million years, and it was too far down the biosynthetic pathway to start creating entirely new antibacterial super-weapons. Besides which, berberine kills bacteria just fine… the problem was that some bacteria evolved a way to get rid it before it accumulates. So what to do? In 2000, researchers Frank Stermitz and his team published the results of a study in which they isolated an innocuous compound from the leaves of Oregon Grape root, called 5′-methoxyhydnocarpin-D (1). It’s a flavonolignan also found in other plant species such as Mimosa diplotricha, and really nothing special or all that sexy. It has no exciting antibiotic properties, and you just might think to ignore it, except that Stermitz et al. discovered that this innocuous chemical binds to the berberine pumps in the bacterial cell wall, effectively disabling them. It was one of the first discoveries of constituent synergism in plants, representing a highly sophisticated adaptation to antibiotic resistance, not by using a bigger or stronger gun, but by using a little trick; or in boxing terms, a right fake and then left to the head that sent the bacteria reeling. Further testing demonstrated that this 1-2 punch combination was effective against antibiotic resistant Staphylococcus (2). Since the publication of this study, a great variety of other natural chemicals have been identified, collectively referred to as multidrug (MDR) efflux inhibitors. These include a broad range of constituents, including the tetrapyrrole pheophorbide A (from Scutellaria barbata); the saponin avenacin A-1 (from Avena sativa); the flavone chrysosplenol-D (from Artemisia annua); the disaccharide neohesperidoside (from Geranium caespitosum); the aromatic ketone chalcone (from Dalea versicolor); the oligosaccharide orizabin (from Ipomoea tricolor); and the indole alkaloid reserpine (from Rauwolfia serpentina) (3). Many researchers are excited about the possibilities of these multidrug (MDR) efflux inhibitors, as this promising new area of research “holds out a great of hope for the development of exciting new drugs”.
<yawn>
Whoops, sorry folks, I must have fell asleep! As I suggested in the first paragraph, the answer is all around us. As a herbalist, I routinely take advantage of the antimicrobial properties of medicinal plants. Why do you think researchers sought to investigate the antimicrobial properties of Oregon grape in the first place? Because it already has a long history of use as a medicinal plant! As we can see, the berberine content only partially explains the antimicrobial properties of Oregon grape; besides berberine there are other bioactive alkaloids in this herb, including the related protoberberine alkaloid jatrorrhizine, as well as a separate group bisbenzylisoquinoline alkaloids including berbamine, oxyacanthine, and tetrandrine, that no doubt contribute the efficacy of berberine. Beyond this tiny grouping isoquinoline alkaloids, however, there are a great many examples of antibacterial chemicals found in other medicinal plants, including those that are active against MRSA, such as emodin (e.g. Aloe spp.), gallic acid (Acacia catechu), glabridin (Glycyrrhiza glabra), punicalagin (Punica granatum), and toralactone (Cassia tora). According to medical experts, however, the reason why modern medicine can’t use herbs is because they don’t contain a sufficiently concentrated source of these antimicrobial compounds, and display too much natural variation. But this is just a myth propagated by the same kind of all-or-none thinking that is characteristic of modern medicine. As the plants show us, we don’t need highly concentrated chemicals to achieve a therapeutic result – we just need the right balance to restore homeostasis. Thus, taking advantage of a medicinal plant’s chemical synergy, herbalists augment this by compounding antimicrobial and complimentary herbs together in different formulas. Although there isn’t very much of any one chemical in a formula, when their additive effect is observed, the result cannot be mistaken. But it’s not like sending in the troops to shut down a rebellion… its more like calling together a neighborhood, a community of constituents, to work collectively for the greater good. In this sense, the herbalist’s approach to infection is really more a form of ecological pruning employed by a diversity of voices, rather than chemical biocide instituted by an authoritarian regime. In my opinion, we should be collectively concerned less with strength and prowess and more with what can we do to restore balance, and leverage the benefit of many small voices to work together as one. It was a certain kind of thinking that got us into this mess, and it’s another type of thinking that will get us out. It doesn’t mean, however, that we can’t use the science to help us, but it should be an informed approach, drawing upon the thousands of years of human experience to guide researchers to look at certain plants over others. For example, in 1992, a research team at UBC published the result of their study which screened 96 species of plants native to British Columbia for in vitro antibiotic activity against eleven bacterial strains (4). Rather surprisingly, the research team found rather that many of the plants which exhibited the strongest antibacterial activity, such the leaves of the wild strawberry (Fragaria chiloensis), weren’t actually used by First Nations for this purpose. Certainly I would never reach for wild strawberry among native plants if I were treating an infection, and I doubt very much this plant would have much success in clinical trials. Such is the importance of context (i.e. extrapolating the results from a test tube study, and attempting to apply this to real life situations). For me ‘context’ is the gold standard when attempting to conduct any research on the therapeutic value of herbal medicine.
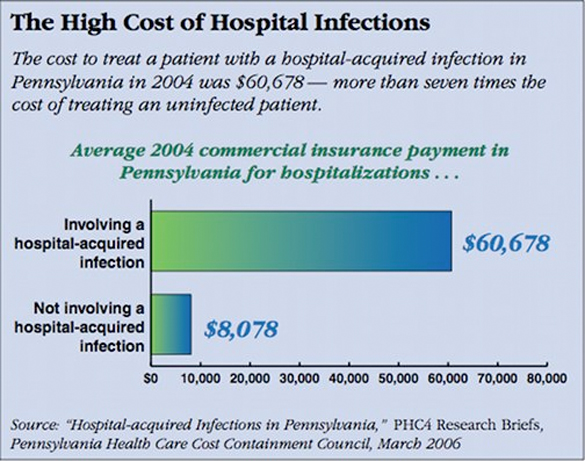
Among the more commonly encountered antibiotic resistant threats is methicillin-resistant Staphylococcus aureus (MRSA). Staphylococcus aureus is a normal part of the human flora, most frequently colonizing the nostrils, but extending outwards from there when the ecological factors favor it, to cause a number of different diseases: from impetigo and boils; to necrotizing pneumonia and infective endocarditis. MRSA is no different from regular Staph except that it is resistant to both the beta-lactam and cephalosporin antibiotics. It most frequently occurs in hospitals (where it originated), as well as in prisons and nursing homes, affecting those with poor hygiene, drug-addiction, immunodeficiency (e.g. aging, cancer, HIV/AIDS), and have open wounds or sores. Although it is easy to blame antibiotics for causing MRSA, the reality is that the ecological factors for virulence are part and parcel of living or working in such institutions. For years health authorities have relied upon housing large groups of sick people in centralized locations, relying upon expensive, proprietary drugs and anti-infectives to maintain a dysfunctional ecology. While many lives have been saved with antibiotics, even despite the way these institutions are managed, the onslaught of these drugs and biocides has resulted in a much bigger, more expensive problem.
Fortunately, there are a great number of herbal extracts and essential oils that are highly effective in the treatment of MRSA and other antibiotic resistant bacteria that can be used to address the issue of antibiotic resistance and drive down health care costs. While many of these natural products haven’t undergone extensive clinical testing, almost all have a long history of use in the treatment of infection, and are being used to this day by practitioners all over the world – including myself. One of the most commonly used antimicrobial herbs in Ayurveda is Neem (Azadirachta indica), traditionally indicated in signs and symptoms of pitta: a class of inflammatory disorders that includes acute infection. In one study, the undiluted oil pressed from Neem fruit exhibited antibacterial activity against 25 strains of multidrug resistant Staphylococcus aureus, Escherichia coli and Pseudomonas aeruginosa isolated from infected patients (5). In another study on Neem, an extract of the leaves was found to exhibit antibacterial, antisecretory and antihemorrhagic activities against drug resistant Vibrio cholerae in experimental animals (6). Similar to Neem is the Ayurvedic herb Bhunimba (Andrographis paniculata), called ‘ground neem’ due to its shared light, dry and bitter properties. Bhunimba has shown a great deal of promise as a therapeutic agent in a variety of disciplines, from virology to oncology, and likewise, has been shown to exhibit antibacterial properties against antibiotic resistant Mycobacterium tuberculosis (7). Other examples of medicinal plants or their essential oils that significantly antibiotic resistance bacteria include Eucalyptus leaf (Eucalyptus globulus), Pomegranate rind (Puncia granatum), Pau D’arco wood (Handroanthus impetiginosus), Amla seed (Phyllanthus emblica), Krishna saireyaka (Acanthus ilicifolius), Olive leaf (Olea europaea), Frankincense resin (Boswellia spp.), and Tea tree leaf (Melaleuca alternifolia). Even common kitchen herbs such as rosemary, thyme, turmeric and garlic have been shown to effectively inhibit a broad range of both gram positive and gram negative multi-drug resistant bacterial species (8, 9, 10, 11).

Considering just how expensive the problem of antibiotic resistance represents to the health care system, I think it very fitting that the solution to antibiotic resistance can be found in something as simple and easy to find as the culinary herbs you eat every day. Who doesn’t have garlic or turmeric on hand? A friend of mine recently demonstrated the utility of such everyday herbs, when he showed me a festering infection he acquired from a stingray incident on the beach. He had already tried antibiotics, but it wasn’t getting better. After looking at it, I told him to douse the wound with freshly ground turmeric powder, cleaning it and changing the dressing a few times a day. Within a week or so, the wound began to heal and resolve without incident. Periodically, when I see him, my friend will remind me of his amazing turmeric experience like it was a big deal. Sometimes I forget to be excited, because I have literally recommended the same or similar approaches to hundreds of people over my 20 years of clinical practice, all with the same results. Hopefully sharing my experience with you on my blog might cause you to reconsider and reframe the problem of antibiotic resistance, and take another look at the natural plant allies all around you. In this way, we can begin to dispense with the fear, and knowing ourselves to be well-supported and fortified by nature, employ our true intelligence and engage in a new dialogue with our bacterial kin, and dispense with the outdated metaphor of war and genocide.
I think it’s about time we grew up as a species, don’t you?


Tumeric ef yeah!
I agree that its about time we grew up as a species!!!
You are gorgeous and intelligent! I wish there were more men like you.
Thank You so much for creating this website!
My daughter and I have been looking for a site like this, with nice pictures of healing herbs and information about them. This is so wonderful!
Have you read The Golden Fountain? It was reading about Piper Longum in that book that led me to look up the herb and find your website thru the link at the bottom of the page for it on Wikipedia. Im so glad I found your site! Thank You Thank You Thank You!
Hi there! I appreciate your article! I am trying to write a research paper for my Master’s program on the bacteria non-resistance to herbs. But I am having trouble locating sources. Could you please post or email me your references? Thanks
I believe all the numbered citations in that piece are hyperlinked – so just click on the number to get the reference!