A couple days ago I blogged on the issue of hypertension and whether it is actually disease. I described it as a self-reinforcing concept that appears to be true, but only if you accept the erroneous premise of the argument. Hypertension, I argued, is not a disease but merely a diagnostic sign, and that by treating a diagnostic sign we mask our ability to monitor the progression of the disease. There are many other diseases in Western medicine that are defined, at least in terms of treatment, not by their symptomology or cause, but by their diagnostic signs.
A similar issue is hyperlipidemia, or ‘high cholesterol’. For years now people have been worried about their cholesterol levels, which like hypertension, is just a simple measurement of a very narrow parameter of physiological function. Like hypertension, you can walk around with elevated cholesterol and not know it. On its own, elevated cholesterol doesn’t cause any problem, and there are no noticeable symptoms. Yet despite this, hyperlipidemia is the defining characteristic of cardiovascular disease. It is, like hypertension, a target of aggressive action, relying on powerful drugs called statins that inhibit cholesterol synthesis (as well as CoQ10, increasing the risk of heart damage).
In terms of research, most of it funded by the pharmaceutical industry, the focus at first was on total serum cholesterol, and then later the types of lipoprotein carriers of cholesterol including VLDL, LDL and HDL. More recently the focus has been on non-cholesterol markers such as lipoprotein(a) and C-reactive protein. The problem is that much of this information is useless, not because it’s not important, but because it becomes a proxy to effective treatment. Drugs are developed to suppress the expression of these different markers in the blood, but not the underlying cause of the disease itself.
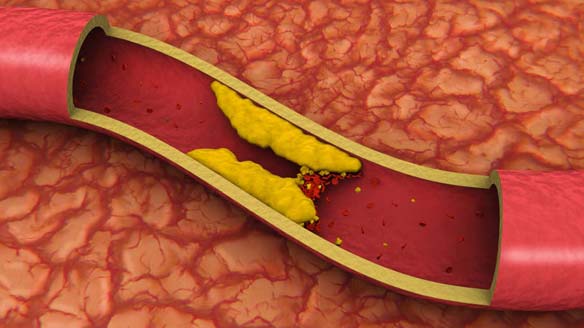
In the case of cholesterol, total serum cholesterol levels actually vary quite widely, and apart from people who have very low cholesterol and die sooner, having statistically higher or lower total serum cholesterol levels doesn’t make that much difference to your risk of dying from heart disease. Thus the notion that all of us should take a drug to lower cholesterol doesn’t make any sense. The HDL:VLDL/LDL ratio is a little more helpful because at least it tells us where the cholesterol is going, either to the periphery of the body (LDL/VLDL) or back to the liver to be recycled (HDL). Restoring the ratio of these lipoproteins however is NOT the intended goal of statins, which is to simply lower cholesterol levels by turning off cholesterol synthesis. Any benefit that statins may have in normalizing lipoprotein ratios seems to be an artifact of an incorrect premise. Likewise, the current thinking that statins “work” not necessarily by lowering cholesterol but because they help to stabilize atherosclerotic plaques is actually more evidence that the cholesterol hypothesis is beginning to break down. But rather than look for a cause, the same approach is being undertaken but this time with different parameters. Wrong drugs like statins are “grandfathered” in to current treatments simply because of the huge business investments that have been made, not because there aren’t very likely hundreds of other cheaper alternatives that will do more or less do the same thing. For example, look at the benefit of fish oil when compared to statins. Despite this fact, new and expensive drugs will continue to be developed all to make the latest diagnostic sign vanish from sight, returning the patient to a steady state of ‘normal’ while the disease continues unchecked. While some might say this approach is illogical, the real issue is that it is an entirely logical business practice called “create the demand”.
Note that I am not denying that cardiovascular disease doesn’t exist. My issue is that “hyperlipidemia” is a best a speculative diagnostic indicator that is being used to good effect by the pharmaceutical industry to give you treatments you don’t need and don’t really work when compared to other options. We need to refocus our efforts, and look at the actual signs and symptoms of cardiovascular disease, and what is happening when total cholesterol and LDL/VLDL goes up. For most people, the primary symptom associated with dyslipidemia is that the person gets fat, mostly around the truncal-abdominal region, i.e. the “love handles”. It can be a little or lot, but most people are generally in tune with their bodies enough to notice when they have any degree of fat accumulation, especially around the belly. The other presenting symptom is that they often feel rather lethargic and heavy, like it’s too difficult to exercise. In Ayurveda, obesity is called medoroga, and it is a precursor disease to prameha, or diabetes. According to Ayurveda, people get fat when they live too softly and eat too much sweet, rich and nourishing foods. Later, this affects circulation and the kidneys, and more complicated signs of cardiovascular disease appear, like angina and worsening glycemic control. But make no mistake: the primary disease is characterized by getting too fat. It can be clearly monitored, and as we get fatter, a whole host of important diagnostic indicators can be found to tell us that things are going wrong. But the disease we are treating is NOT elevated cholesterol, elevated LDL/VLDLD, elevated lipoprotein-A or elevated C-reaction protein. It is impaired metabolic function: that is the disease we should be focused on.
As for cholesterol itself, and why it might be elevated in cardiovascular disease, let’s look to what we know about cholesterol. Apart from forming the structure of important steroid hormones (e.g. testosterone, estrogen etc) and vitamin D3, cholesterol acts as a membrane-stabilizing molecule and antioxidant. Essentially, the body uses cholesterol to inhibit inflammation in the cell membrane, something we have known for years. Cell biology 101. But why is the body synthesizing cholesterol and depositing it in the artery? Inflammation. Very clearly we know that it’s inflammation, with markers like C-reactive protein to indicate this. But if the body is synthesizing cholesterol to stabilize inflammation, why do we want to inhibit its ability to heal the endothelial lining by suppressing cholesterol synthesis with statins? Beyond its weak benefits in plaque stabilization, what justifies leaving the body without any cholesterol to stop the inflammation? How is this a good idea?
If your weight and cholesterol levels go up, and lipoprotein levels get wonky, you should know that there is inflammation in your vascular system. If this is the case, undertake a serious inventory in your life and ask yourself if you’ve become too soft, too inactive, and if there’s too much inertia in your life. If so, it’s time to re-activate your health. Many things will cause inflammation in your body: tobacco, stress, infection, poor digestion, nutrient deficiencies, immune dysfunction, and environmental toxins. All of these are important but the primary factor involved in endothelial inflammation is chronically elevated blood sugar, leading to elevated insulin levels and insulin resistance. There’s lots of research to show how elevated blood sugar directly damages endothelial proteins through a process called non-enzymatic glycation, resulting in blood vessel inflammation. All of this leads to the inevitable conclusion that cardiovascular disease is in large part a disease of excess sweet. Interestingly, sweet is a flavor in Ayurveda which acts to comfort, pacify, soothe and nourish the body. Excess sweet creates fat which leads to obesity, which as we know is defined as a disease of soft living. Thus to heal your vascular system, look at the quality of sweetness in your life, and rather than food, find it in other places, like maybe a hug or kiss, or maybe a nice massage. Resolve to live a little tougher, and shed those pounds fed by soft-living. If you start doing this, you just might find that you never really needed blood-pressure lowering drugs or statins in the first place.